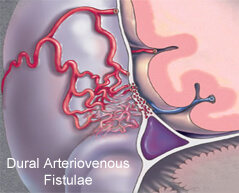
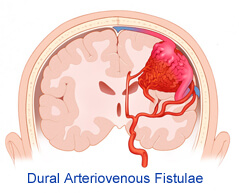
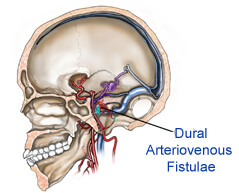
Dural Arteriovenous Fistulae
Dural arteriovenous fistulas are abnormal connections between an artery and the tough covering over the brain or spinal cord (dura) and a draining vein. Abnormal passageways between arteries and veins (arteriovenous fistulas) may occur in the brain, spinal cord or other areas of your body.
Borden Classification
 The Borden Classification of dural arteriovenous malformations or fistulas, groups into three types based upon their venous drainage:
The Borden Classification of dural arteriovenous malformations or fistulas, groups into three types based upon their venous drainage:
Type I: dural arterial supply drains anterograde into venous sinus.
Type II: dural arterial supply drains into venous sinus. High pressure in sinus results in both anterograde drainage and retrograde drainage via subarachnoid veins.
Type III: dural arterial supply drains retrograde into subarachnoid veins.
Type I
Type I dural arteriovenous fistulas are suppied by meningeal arteries and drain into a meningeal vein or dural venous sinus. The flow within the draining vein or venous sinus is anterograde.
Type Ia - simple dural arteriovenous fistulas have a single meningeal arterial supply
Type Ib - more complex arteriovenous fistulas are supplied by multiple meningeal arteries
The distinction between Types Ia and Ib is somewhat specious as there is a rich system of meningeal arterial collaterals. Type I dural fistulas are often asymptomatic, do not have a high risk of bleeding and do not necessarily need to be treated.
Type II
The high pressure within a Type II dural AV fistula causes blood to flow in a retrograde fashion into subarachnoid veins which normally drain into the sinus. Typically this is because the sinus has outflow obstruction. Such draining veins form venous varices or aneurysms which can bleed. Type II fistulas need to be treated to prevent hemorrhage. The treatment may involve embolization of the draining sinus as well as clipping or embolization of the draining veins.
Type III
Type III dural AV fistulas drain directly into subarachnoid veins. These veins can form aneurysms and bleed. Type III dural fistulas need to be treated to prevent hemorrhage. Treatment can be as simple as clipping the draining vein at the site of the dural sinus. If treatment involves embolization, it will only typically be effective if the glue traverses the actual fistula and enters, at least slightly, the draining vein.

Planning your medical trip to India is a very simple process with Spine and Neuro Surgery Hospital India
- You just need to fill in our enquiry form and one of our executive will contact you soon.
- +91-9325887033 Call us at the given to contact number for any assistance.
- Complete information regarding surgery is provided on our website.
Cognard Classification
The Cognard Classification[3] correlates venous drainage patterns with increasingly aggressive neurological clinical course.
Type I
 Confined to sinus wall, typically after thrombosis.
Confined to sinus wall, typically after thrombosis.
Type II
IIa - confined to sinus with reflux (retrograde) into sinus but not cortical veins. IIb - drains into sinus with reflux (retrograde) into cortical veins (10-20% hemorrhage).
Type III
Drains direct into cortical veins (not into sinus) drainage (40% hemorrhage).
Type IV
Drains direct into cortical veins (not into sinus) drainage with venous ectasia (65% hemorrhage).
Type V
Spinal perimedullary venous drainage, associated with progressive myelopathy.
Dural arteriovenous fistulas are fistulas connecting the branches of dural arteries to dural veins or a venous sinus. Digital subtraction angiography remains the gold standard for diagnosing these fistulas. Endovascular treatment is one of the first line options available for their management. This review article reviews the etiopathogenesis, natural history, common classification systems and various available treatment options.
Yasargill noted that Rizzoli, in 1881, was the first to describe an arteriovenous malformation (AVM) that involved the dura mater and Sachs reported the first, angiographic description in 1931. Subsequently cranial dural fistulas have been most frequently described at the transverse sinus and cavernous sinus, although they occur at every cranial dural sinus. Dural arteriovenous fistulas (DAVFs) can occur anywhere within the intracranial dura mater. DAVFs are rare vascular abnormalities. They consist of numerous tiny connections between branches of dural arteries and veins or a venous sinus. The true incidence of DAVFs is unknown. However, the reported incidence of intracranial DAVFs is approximately 10-15% of all intracranial vascular abnormalities. A good percentage of DAVFs remain clinically silent or involute spontaneously and therefore the true incidence may be much more.[3] Present evidence suggests that DAVFs are acquired lesions and present later in life than AVMs.
Etiopathology
Before the mid-1970s DAVFs were thought to be congenital in origin and to be associated with other vascular lesions. In the late 1970s, Castaigne and Djindjian proposed an acquired etiology. They suggested that DAVFs may develop due to the opening up of existing micro shunts within the dura and by angioneogenesis, leading to the development of new shunts. Various etiologies are postulated: e.g., anomalies of venous system, venous thrombosis, head trauma, transcranial surgery, association with pregnancy, delivery and menopause, increased systemic thrombotic activity, cortical vein thrombosis (CVT), role of hormonal changes (use of oral contraceptive and pregnancy) causing increased angiogenesis, tumors (meningiomas obstruct dural venous outflow), general surgery, otitis, and sinusitis.[5]
Understanding of the pathophysiology of DAVFs came from the school of La Salpetriere, which emphasized the role of the cortical venous drainage of these dural shunts.[5] Henceforth, the role of the subarachnoid and subpial venous drainage could be correlated with the type of neurological manifestation and the natural history of dural shunts. Conditions associated with DAVFs include stenosis or occlusion of the draining dural sinuses, sinus thrombosis, prothrombin gene mutation, resistance to activated protein (APCR), mutation in factor V gene, and presence of antiphospholipid antibodies.
 DAVFs in adulthood are an acquired disease and there is no relationship to hereditary or developmental disorders. On the other hand, we have seen brain AVMs as well as cavernomas occur in patients with DAVFs. Vascular diseases associated with dural arteriovenous shunts include cerebral AVM, maxillofacial AVM, hereditary hemorrhagic telangiectasia, bone AVM, cavernomas, and intradural or extradural arterial aneurysms. Multiple DAVFs at separate locations in the same patient have also been reported. The common predisposing factor for DAVFs appears to be venous sinus thrombosis. The venous hypertension developing after venous thrombosis opens up the microvascular connections within the dura. Without intervention, these channels become hypertrophied resulting in direct shunting between the arteries and veins . When the fistula grows and becomes more diffuse, it recruits pial supply from parenchymal vessels. This may lead to the angiomatous network of multiple feeding arteries and numerous AV shunts within a partially recanalized sinus that is frequently seen at angiography. The involved dural sinus receives arterialized blood flow that can lead to mechanical obstruction of the sinus and result in retrograde drainage of blood away from the sinus and into the cortical veins. Histopathological analysis of excised DAVFs has revealed thrombosis and angiographic progression of sinus thrombosis to DAVF. In addition, dilatation of the cortical veins may occur, predisposing the patient to intracranial hemorrhage.
DAVFs in adulthood are an acquired disease and there is no relationship to hereditary or developmental disorders. On the other hand, we have seen brain AVMs as well as cavernomas occur in patients with DAVFs. Vascular diseases associated with dural arteriovenous shunts include cerebral AVM, maxillofacial AVM, hereditary hemorrhagic telangiectasia, bone AVM, cavernomas, and intradural or extradural arterial aneurysms. Multiple DAVFs at separate locations in the same patient have also been reported. The common predisposing factor for DAVFs appears to be venous sinus thrombosis. The venous hypertension developing after venous thrombosis opens up the microvascular connections within the dura. Without intervention, these channels become hypertrophied resulting in direct shunting between the arteries and veins . When the fistula grows and becomes more diffuse, it recruits pial supply from parenchymal vessels. This may lead to the angiomatous network of multiple feeding arteries and numerous AV shunts within a partially recanalized sinus that is frequently seen at angiography. The involved dural sinus receives arterialized blood flow that can lead to mechanical obstruction of the sinus and result in retrograde drainage of blood away from the sinus and into the cortical veins. Histopathological analysis of excised DAVFs has revealed thrombosis and angiographic progression of sinus thrombosis to DAVF. In addition, dilatation of the cortical veins may occur, predisposing the patient to intracranial hemorrhage.
Another mechanism for DAVF evolution is the release of angiogenic growth factors such as vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF), which promotes neovascularization and development of a DAVF [Tables 2 and 3]. These factors by themselves should therefore not be considered as the direct cause of DAVFs, but rather they make up an environment that may be conducive to the development of DAVF, depending on the individual host response to their presence. DAVF in adults are triggered by factors that stimulate angiogenesis. If this angiogenic process is simultaneously associated with loss of some of the venular surface properties, then venous thrombosis is likely to occur. It has been noted that angiogenic growth factors such as basic fibroblast growth factor (bFGF) and vascular endothelial growth factor (VEGF) are expressed in the DAVFs. In DAVFs with a patent sinus, cortical venous pathways usually do not develop and hemorrhagic complications with these DAVFs are infrequent.
Hospitals such as hospital in Nagpur provide specialized treatment for Neuro treatment. The cost of surgery is comparatively quite low in Spine and Neuro Surgery Hospital.
Get Low Cost Dural Arteriovenous Fistulae Surgery in India
We offer free assistance to international patients to find best medical treatment in India. We offer low-cost, world-class medical treatment in India, coordinated by a team of experienced service industry professionals
Please post a query to know about low cost treatment options at top India hospitals
Click Here
