Arteriovenous Malformation (AVM)
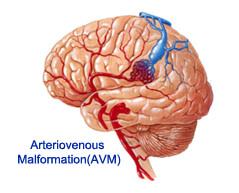
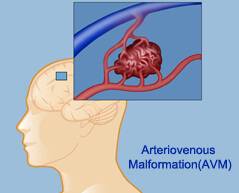 A brain (intracranial) arteriovenous malformation (AVM) is an abnormal tangle of arteries and veins in your brain. These are congenital lesions, meaning that they can develop before you're born. Arteriovenous malformations can also occur in your spinal cord (spinal arteriovenous malformation).
A brain (intracranial) arteriovenous malformation (AVM) is an abnormal tangle of arteries and veins in your brain. These are congenital lesions, meaning that they can develop before you're born. Arteriovenous malformations can also occur in your spinal cord (spinal arteriovenous malformation).
Oxygen-rich blood normally enters your brain through arteries, which branch into smaller arterioles and even smaller blood vessels (capillaries). Your brain uses oxygen removed from the blood in your capillaries. Oxygen-depleted blood then passes into small venules and then into larger veins that drain the blood from your brain to your heart and lungs.

Planning your medical trip to India is a very simple process with Spine and Neuro Surgery Hospital India
- You just need to fill in our enquiry form and one of our executive will contact you soon.
- +91-9325887033 Call us at the given to contact number for any assistance.
- Complete information regarding surgery is provided on our website.
A brain AVM (arteriovenous malformation) is an abnormal connection between arteries and veins. An AVM is usually congenital, meaning it dates to birth.
An AVM can develop anywhere in your body but occurs most often in the brain or spine. A brain AVM, which appears as a tangle of abnormal arteries and veins, can occur in any part of your brain. The cause isn't clear.
You may not know you have a brain AVM until you experience symptoms, such as headaches or a seizure. In serious cases, the blood vessels rupture, causing bleeding in the brain (hemorrhage). Once diagnosed, a brain AVM can often be treated successfully.
A brain AVM (arteriovenous malformation) may not cause any signs or symptoms until the AVM ruptures, resulting in bleeding in the brain (hemorrhage). However, some people with an AVM may have symptoms other than bleeding that are related to the AVM.
An AVM may also be detected on a brain scan performed for reasons unrelated to the AVM.
Get Low Cost Arteriovenous Malfunction Treatment from TOP Hospitals in India
We offer free, no obligation assistance to international patients to find best Embolization AVM Surgery in India. We offer low-cost, world-class Embolization AVM Surgery in India, coordinated by a team of experienced service industry professionals
Please post a query to know about low cost treatment options at top India hospitals
Click Here
Symptoms of a brain AVM include:
- Seizures
- A whooshing sound (bruit) that can be heard on examination of the skull with a stethoscope or may be audible if you have an AVM
- Headache
- Progressive weakness or numbness
- Some people may experience more-serious neurological symptoms, depending on the location of the AVM, including:
- Severe headache
- Weakness, numbness or paralysis
- Vision loss
- Difficulty speaking
- Inability to understand others
- Severe unsteadiness
Symptoms may begin at any age, but you're more likely to experience symptoms between ages 10 and 40. Brain AVM can damage brain tissue over time. The effects slowly build up, sometimes causing symptoms in early adulthood.
Once you reach middle age, however, brain AVMs tend to remain stable and are less likely to cause symptoms. Some pregnant women may have worsened symptoms. However, it's not clear that pregnant women are at greater risk of an AVM bleeding. More research is needed to determine the risk during pregnancy.
.jpg) In a brain arteriovenous malformation, your blood passes directly from your arteries to your veins, bypassing capillaries. The arteries and veins in an AVM can rupture, causing bleeding into the brain.
In a brain arteriovenous malformation, your blood passes directly from your arteries to your veins, bypassing capillaries. The arteries and veins in an AVM can rupture, causing bleeding into the brain.
Arteriovenous malformations (AVMs) are congenital lesions composed of a complex tangle of arteries and veins connected by one or more fistulae. They most commonly occur in young adults, with morbidity and death occurring in 30-50% and 10-15% of patients, respectively.
Signs and symptoms
Considerations regarding patient history include the following:
AVMs tend to be clinically silent until the presenting event occurs; therefore, the diagnosis usually is made at the time of the first seizure or hemorrhage
A history of minor learning disability is found in as many as two thirds of patients; such dysfunction is rarely apparent in adult life
A history of headaches is found in as many as half of all patients with cerebral AVM; the headaches subsequently may take the form of classic migraine or more generalized headache
If seizures have occurred, a careful seizure history should be obtained; seizures are simple, partial, or secondarily generalized
Physical examination
Considerations regarding the physical examination of patients with AVM include the following:
Focal neurologic findings are rare in the absence of seizure or hemorrhage in patients with cerebral AVMs; they are more common in AVMs that are deeply located or in the brainstem
Detailed neuropsychological testing may disclose subtle right or left hemisphere dysfunction
If parenchymal hemorrhage is present, the physical findings are indistinguishable from those produced by intracranial hemorrhage from other causes
Intraventricular hemorrhage generally produces a less severe neurologic deficit than does hemorrhage into other areas of the brain
In the rare patients in whom focal neurologic deficits are present, the deficit may reflect the location of the AVM The following imaging studies are used in the diagnosis and assessment of cerebral AVM:
Computed tomography (CT) scanning: Easily identifies intracerebral hemorrhages, raising suspicion of AVM in a younger person or a patient without clear risk factors for hemorrhage; however, this modality can identify only large AVMs.
Magnetic resonance imaging (MRI): Essential for the initial diagnosis of AVMs; the malformations appear as irregular or globoid masses anywhere within the hemispheres or brainstem; a retrospective analysis demonstrated that silent intralesional microhemorrhage on CT scan/MRI may be a risk factor for intracerebral hemorrhage from a brain AVM rupture[1]
Cerebral angiography: Required for hemodynamic assessment, which is essential for planning treatment Superselective angiography: Performed with standard cerebral angiography, with access via a femoral artery puncture Invasive treatment is recommended for younger patients with 1 or more high-risk features for an AVM rupture. Older individuals and patients with no high-risk features may be best treated through management of the medical aspects of the illness alone; in such patients, anticonvulsants for seizure control and appropriate analgesia for headaches may be the only treatment recommendations necessary.
Invasive treatment of AVMs may include endovascular embolization, surgical resection, and focal beam radiation, alone or in any combination. The current American Heart Association multidisciplinary management guidelines for the treatment of brain AVMs recommend the following approach:[2]
Surgical extirpation is strongly suggested as the primary treatment for AVMs of Spetzler-Martin grade I or II if they are surgically accessible with low risk
Radiation therapy alone is recommended for AVMs of Spetzler-Martin grade I or II if they are less than 3 cm in size and surgery has an increased surgical risk based on location and vascular anatomy
Brain AVMs of Spetzler-Martin grade III can often be treated with a multimodal approach that uses embolization followed by surgical extirpation. If the lesion has a high surgical risk based on location and vascular anatomy, radiation therapy may be performed after embolization
Hospitals such as hospital in Nagpur provide specialized treatment for Neuro treatment. The cost of surgery is comparatively quite low in Spine and Neuro Surgery Hospital.
 AVMs of Spetzler-Martin grade IV or V are often not amenable to surgical treatment alone because of the high procedural risk; these AVMs can be treated using a combined multimodal approach that includes embolization, radiosurgery, and/or surgery
AVMs of Spetzler-Martin grade IV or V are often not amenable to surgical treatment alone because of the high procedural risk; these AVMs can be treated using a combined multimodal approach that includes embolization, radiosurgery, and/or surgery
In general, embolization should be performed only if the goal is complete AVM eradication with other treatment modalities; the only exception is palliative embolization in patients with an AVM of Spetzler-Martin grade IV or V with venous outflow obstruction or true steal phenomenon, in order to reduce arterial inflow to control edema or to reduce the amount of shunt, respectively.
Treatment planning for AVMs depends on risk of subsequent hemorrhage, which is determined by the demographic, historical, and angiographic features of the individual patient as discussed above. Prior hemorrhage, smaller AVM size, deep venous drainage, and relatively high arterial feeding pressures make subsequent hemorrhage more likely.
What services we offer to our International Patient?
- Straight forward - simple booking procedure to seek top Medical Treatmentin India.
- Full assistance to get Medical Visa.
- Low cost - a fraction of the cost of UK/USA surgery.
- Low risk - world's highest standards of clinical care & surgery.
- Fast efficient service - immediate treatment with no waiting lists.
- Full patient support service - 24/7 services.
- Specialist consultations - scans, clinical investigations & consultations at short notice.
- Individual time to each patient
- Patients without insurance are equally benefitted
- Provides the world’s highest standards of clinical care & surgery.
- Receive the travelers at the airport
- Keep track of the additional requirements (if discovered during the treatment) and organize interventions accordingly to strive to ensure that the treatment process does not get disrupted.
- Handhold the travelers during their shopping/sight-seeing tours - we may or may accompany the travelers, but we coordinate for a smooth and pleasurable experience (at extra cost)
- In case the patient/attendant are English-constrained, then provide interpreter services Quick response and availability of revert.
- Visible compassion for the traveler.
Patient Testimonial – Ms. Adel Mitchell from Newzealand sharing her experience of Arteriovenous Malformation Treatment done in India

Ms. Adel Mitchell from Newzealand
I was having continuous headaches since months. In fact, they were affecting my sleep and I was finding it difficult to concentrate in my work too. It was really depressing to feel sick all the time. That’s when I consulted the doctors of spine and neuro surgery group and they were very thorough with my diagnosis. They always explained me about the procedure that they were going to follow for arteriovenous malformation treatment. Even the staff members in the hospital are so friendly that I didn’t feel alone or depressed during the process. There has been a dramatic improvement since the surgery.
How to plan your medical trip to India?
- Send us your query and medical reports
- Get the advised opinion and treatment plan from us within 48 hours from multiple hospitals
- Choose your preferred hospital and clear your concerns if you have any
- We will assist you with medical VISA, Vaccination, FRRO, Travel, Accommodation and Logistic Process
- Arrival arrangements will be done for your pick up at the airport based on your itinerary
- Treatment will start at the hospital as planned
- Once the treatment is done, you can fly back
- Post treatment follow up and consultation will be done by us via email, phone, Skype
